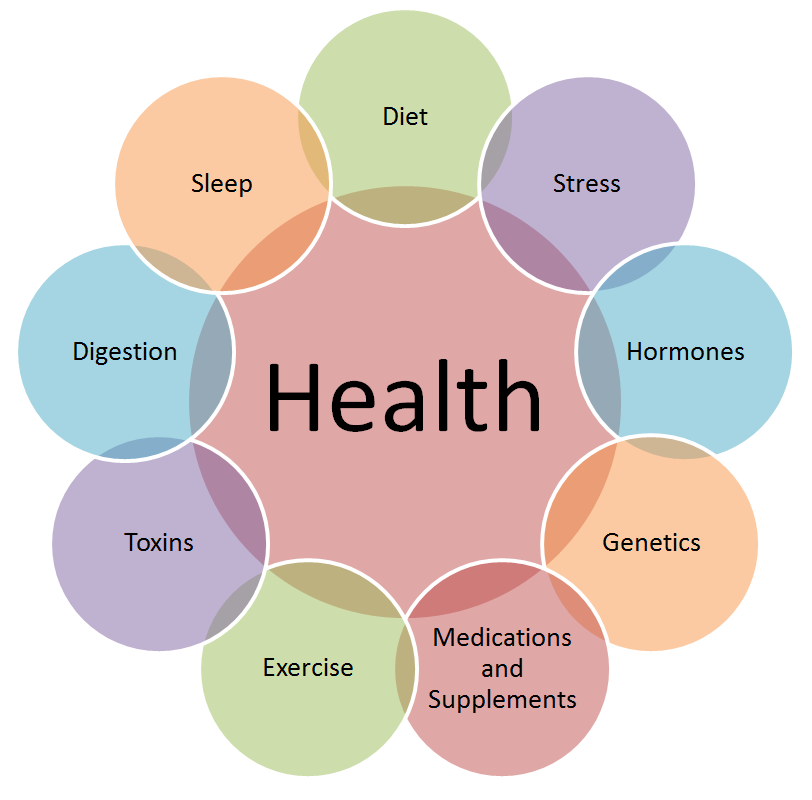
In recent years, the gut has earned the title of the “second brain” due to its profound influence on overall health. Beyond digestion, the gut plays a pivotal role in regulating hormones, which in turn affects weight management. As a functional medicine practitioner, I’ve seen firsthand how optimizing gut health can transform lives, especially for those struggling with hormonal imbalances and weight loss. In this article, we’ll explore the intricate connection between gut health, hormone regulation, and weight loss, and provide actionable steps to improve your gut health for better overall well-being.
The Gut-Hormone Connection: A Complex Relationship
The gut is home to trillions of microorganisms, collectively known as the gut microbiome. These microbes are not just passive residents; they actively communicate with the body’s endocrine system, which is responsible for hormone production and regulation. Here’s how the gut influences hormones:
- Production of Key Hormones: The gut microbiome produces and modulates hormones such as serotonin, dopamine, and ghrelin. For example, about 90% of serotonin, the “feel-good” hormone, is produced in the gut. Imbalances in serotonin levels can lead to mood disorders, cravings, and overeating.
- Regulation of Insulin: A healthy gut helps regulate blood sugar levels by influencing insulin sensitivity. An imbalanced gut microbiome can lead to insulin resistance, a key factor in weight gain and metabolic disorders like type 2 diabetes.
- Estrogen Metabolism: The gut microbiome plays a crucial role in metabolizing estrogen. An unhealthy gut can lead to estrogen dominance, which is associated with weight gain, bloating, and hormonal imbalances.
- Cortisol and Stress Response: The gut-brain axis connects the gut and the brain, influencing the body’s stress response. Chronic stress can disrupt gut health, leading to elevated cortisol levels, which promote fat storage, particularly around the abdomen.
How Gut Health Impacts Weight Loss
Weight loss is not just about calories in versus calories out. Hormonal imbalances, often rooted in poor gut health, can sabotage even the most disciplined diet and exercise plans. Here’s how your gut health influences weight loss:
- Appetite Regulation: The gut produces hormones like ghrelin (hunger hormone) and leptin (satiety hormone). An imbalanced gut can disrupt these hormones, leading to increased appetite, cravings, and overeating.
- Nutrient Absorption: A healthy gut ensures proper absorption of nutrients, which are essential for metabolism and energy production. Poor gut health can lead to nutrient deficiencies, slowing down metabolism and making weight loss more challenging.
- Inflammation and Fat Storage: An unhealthy gut can trigger chronic inflammation, which is linked to obesity. Inflammation disrupts hormone signaling, leading to increased fat storage, particularly visceral fat.
- Microbiome Diversity: Studies show that individuals with a diverse gut microbiome are more likely to maintain a healthy weight. A lack of microbial diversity is associated with obesity and metabolic disorders.
Signs Your Gut Health May Be Affecting Your Hormones and Weight
If you’re struggling with weight loss or hormonal imbalances, your gut health could be the culprit. Here are some common signs of poor gut health:
- Persistent bloating, gas, or indigestion
- Frequent sugar or carb cravings
- Unexplained weight gain or difficulty losing weight
- Mood swings, anxiety, or depression
- Irregular menstrual cycles or PMS symptoms
- Fatigue or low energy levels
If you’re experiencing any of these symptoms, it’s time to prioritize your gut health.
Five Actionable Steps to Improve Gut Health for Hormone Regulation and Weight Loss
- Eat a Fiber-Rich Diet: Fiber feeds the beneficial bacteria in your gut, promoting a healthy microbiome. Include plenty of fruits, vegetables, legumes, and whole grains in your diet. Fermented foods like yogurt, kefir, sauerkraut, and kimchi are also excellent for gut health.
- Prioritize Probiotics and Prebiotics: Probiotics are live beneficial bacteria, while prebiotics are the food that feeds them. Incorporate probiotic-rich foods like yogurt and kombucha, and prebiotic-rich foods like garlic, onions, and bananas.
- Reduce Stress: Chronic stress wreaks havoc on your gut and hormones. Practice stress-reducing techniques like meditation, yoga, deep breathing, or spending time in nature.
- Avoid Gut Irritants: Processed foods, sugar, artificial sweeteners, and excessive alcohol can harm your gut lining and disrupt your microbiome. Opt for whole, unprocessed foods instead.
- Stay Hydrated: Water is essential for digestion and maintaining the mucosal lining of the gut. Aim for at least 8 glasses of water daily.
The Role of Functional Medicine in Gut Health and Hormone Balance
As a functional medicine practitioner, I take a holistic approach to gut health and hormone regulation. This involves:
- Comprehensive Testing: Identifying gut imbalances through stool tests, hormone panels, and food sensitivity tests.
- Personalized Nutrition Plans: Tailoring diets to support gut health and hormone balance.
- Lifestyle Modifications: Addressing stress, sleep, and exercise to optimize overall health.
- Targeted Supplementation: Using probiotics, digestive enzymes, and other supplements to restore gut health.
Success Story: Transforming Health Through Gut Healing
One of my patients, Sarah, struggled with weight gain, fatigue, and irregular periods for years. After comprehensive testing, we discovered she had gut dysbiosis (an imbalance in her gut microbiome) and estrogen dominance. Through a personalized gut-healing protocol, including dietary changes, probiotics, and stress management, Sarah not only lost 25 pounds but also regained her energy and balanced her hormones. Her story is a testament to the power of addressing gut health for overall well-being.
Conclusion: Your Gut Holds the Key to Hormonal Balance and Weight Loss
The gut is far more than a digestive organ; it’s a central player in hormone regulation and weight management. By prioritizing gut health, you can address the root cause of hormonal imbalances and achieve sustainable weight loss. Remember, small, consistent changes can lead to significant improvements over time. If you’re ready to take control of your health, start by nurturing your gut today.
Dr. Zaar is a functional medicine practitioner specializing in gut health, hormone balance, and weight management. With over a decade of experience, he has helped countless patients achieve optimal health through personalized, holistic approaches.
If you learn more about Gut Health, Please Visit the drzaar.com