Testosterone is a vital hormone in the human body, playing a crucial role in muscle mass, bone density, mood regulation, and sexual health. However, as men age, testosterone levels naturally decline, leading to a condition known as testosterone deficiency or hypogonadism. This condition can significantly impact quality of life, but the good news is that it is manageable with proper diagnosis and treatment. In this article, we’ll explore the causes, symptoms, and treatment options for testosterone deficiency, providing you with the knowledge to take control of your health.
What is Testosterone Deficiency?
Testosterone deficiency occurs when the body fails to produce adequate levels of testosterone, the primary male sex hormone. While it is more common in older men, younger men can also experience low testosterone due to various factors. The condition can lead to a range of physical, emotional, and sexual symptoms, making early diagnosis and treatment essential.
Causes of Testosterone Deficiency
Several factors can contribute to low testosterone levels. Understanding these causes can help in identifying the root of the problem and seeking appropriate treatment.
- Aging: Testosterone levels peak during early adulthood and gradually decline by about 1% per year after the age of 30.
- Medical Conditions: Conditions such as obesity, diabetes, and metabolic syndrome can negatively impact testosterone production.
- Injury or Infection: Damage to the testicles or infections in the reproductive system can affect hormone production.
- Hormonal Disorders: Disorders of the pituitary gland or hypothalamus can disrupt the signals that stimulate testosterone production.
- Lifestyle Factors: Poor diet, lack of exercise, excessive alcohol consumption, and chronic stress can all contribute to low testosterone levels.
Symptoms of Testosterone Deficiency
The symptoms of low testosterone can vary widely, but they often include:
- Physical Symptoms:
- Reduced muscle mass and strength
- Increased body fat, particularly around the abdomen
- Fatigue and low energy levels
- Decreased bone density, leading to a higher risk of fractures
- Emotional Symptoms:
- Mood swings, irritability, and depression
- Difficulty concentrating and memory problems
- Sexual Symptoms:
- Reduced libido (sex drive)
- Erectile dysfunction
- Decreased semen production
If you’re experiencing any of these symptoms, it’s important to consult a healthcare professional for a proper diagnosis.
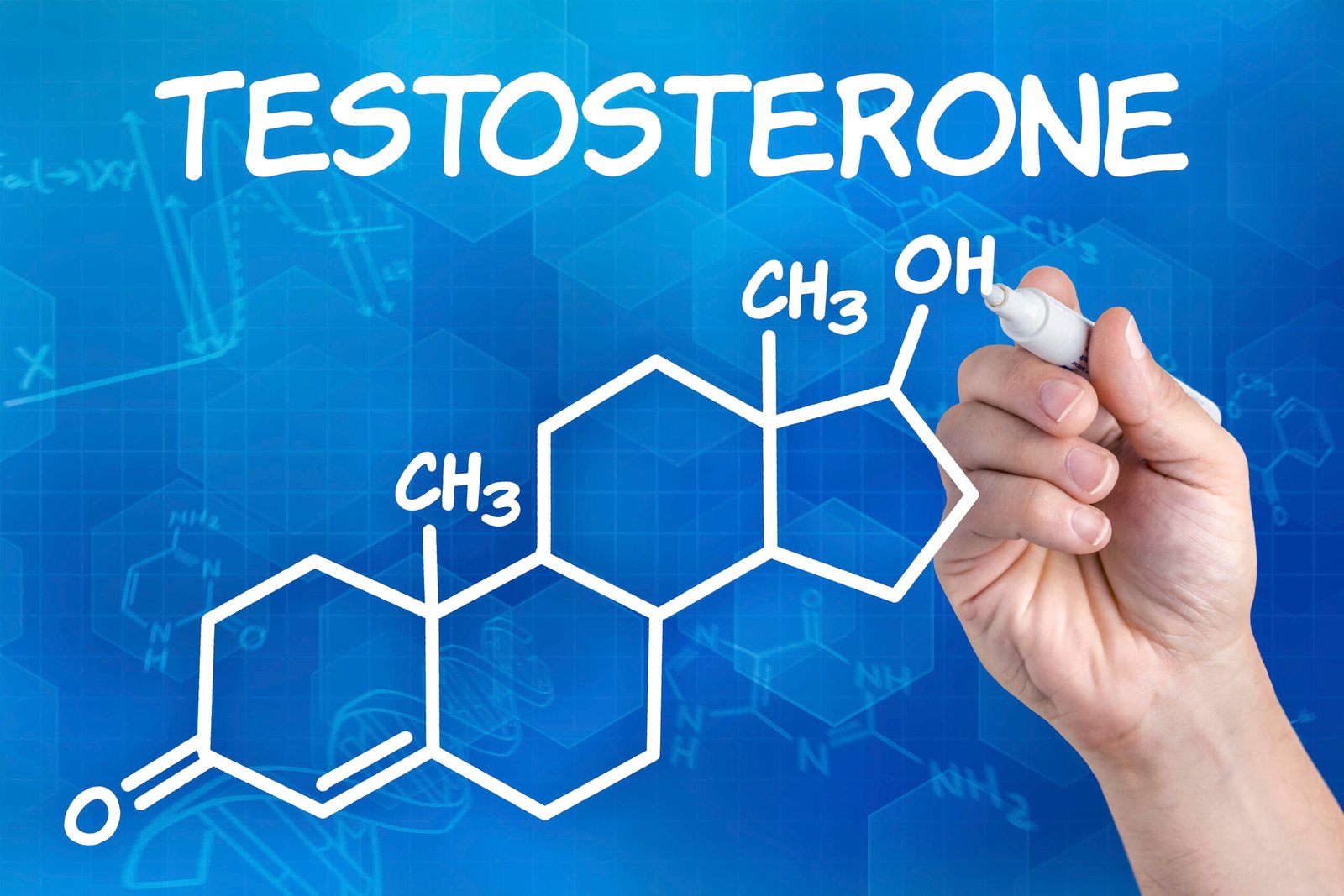
Diagnosing Testosterone Deficiency
Diagnosing low testosterone involves a combination of symptom assessment and blood tests. A healthcare provider will typically measure total testosterone levels, which should ideally be between 300 and 1,000 nanograms per deciliter (ng/dL). Levels below this range may indicate testosterone deficiency.
In some cases, additional tests may be required to determine the underlying cause of low testosterone, such as measuring luteinizing hormone (LH) and follicle-stimulating hormone (FSH) levels.
Treatment Options for Testosterone Deficiency
Once diagnosed, there are several treatment options available to manage testosterone deficiency effectively. The choice of treatment depends on the severity of the condition, the underlying cause, and the patient’s preferences.
- Testosterone Replacement Therapy (TRT):
TRT is the most common treatment for low testosterone. It involves supplementing the body with synthetic testosterone through:- Injections: Testosterone can be injected directly into the muscles every 1-2 weeks.
- Gels and Patches: Topical applications allow testosterone to be absorbed through the skin.
- Implants: Small pellets are inserted under the skin, releasing testosterone over several months.
While TRT can be highly effective, it is not without risks. Potential side effects include acne, sleep apnea, and an increased risk of blood clots. Regular monitoring by a healthcare provider is essential to ensure safe and effective treatment.
- Lifestyle Changes:
In some cases, making lifestyle changes can help boost testosterone levels naturally. These include:- Exercise: Regular physical activity, especially strength training, can stimulate testosterone production.
- Diet: A balanced diet rich in protein, healthy fats, and essential nutrients supports hormonal health.
- Sleep: Adequate sleep is crucial for hormone regulation.
- Stress Management: Reducing stress through mindfulness, meditation, or therapy can improve testosterone levels.
- Medications:
Certain medications, such as clomiphene citrate, can stimulate the body’s natural production of testosterone. These are often used as an alternative to TRT, particularly in younger men who wish to preserve fertility. - Addressing Underlying Conditions:
If low testosterone is caused by an underlying medical condition, such as obesity or diabetes, treating that condition can help restore normal hormone levels.
Risks and Considerations
While treatment for testosterone deficiency can be highly effective, it’s important to weigh the benefits against the potential risks. For example, TRT may not be suitable for men with a history of prostate cancer or severe heart disease. Additionally, long-term use of TRT can lead to a reduction in natural testosterone production.
It’s crucial to work closely with a healthcare provider to develop a personalized treatment plan that addresses your specific needs and concerns.
Preventing Testosterone Deficiency
While some factors, such as aging, are beyond our control, there are steps you can take to maintain healthy testosterone levels:
- Maintain a healthy weight through diet and exercise.
- Avoid excessive alcohol consumption and smoking.
- Manage stress through relaxation techniques and self-care.
- Get regular check-ups to monitor hormone levels and overall health.
Conclusion
Testosterone deficiency is a common but often overlooked condition that can significantly impact quality of life. By understanding the causes, symptoms, and treatment options, you can take proactive steps to manage your health and well-being. Whether through testosterone replacement therapy, lifestyle changes, or addressing underlying conditions, effective treatment is within reach.
If you suspect you may have low testosterone, don’t hesitate to seek medical advice. Early diagnosis and treatment can make all the difference in restoring your energy, vitality, and overall health.
If you learn more about Testosterone, Please visit the drzaar.com