In today’s fast-paced world, maintaining a strong immune system is more important than ever. Your immune system is your body’s natural defense mechanism against infections, viruses, and diseases. A robust immune system not only helps you fight off illnesses but also ensures you stay energetic and healthy. But how can you boost your immune system naturally? In this article, we’ll explore proven strategies and tips to strengthen your immunity, backed by science and expert advice.
Understanding the Immune System
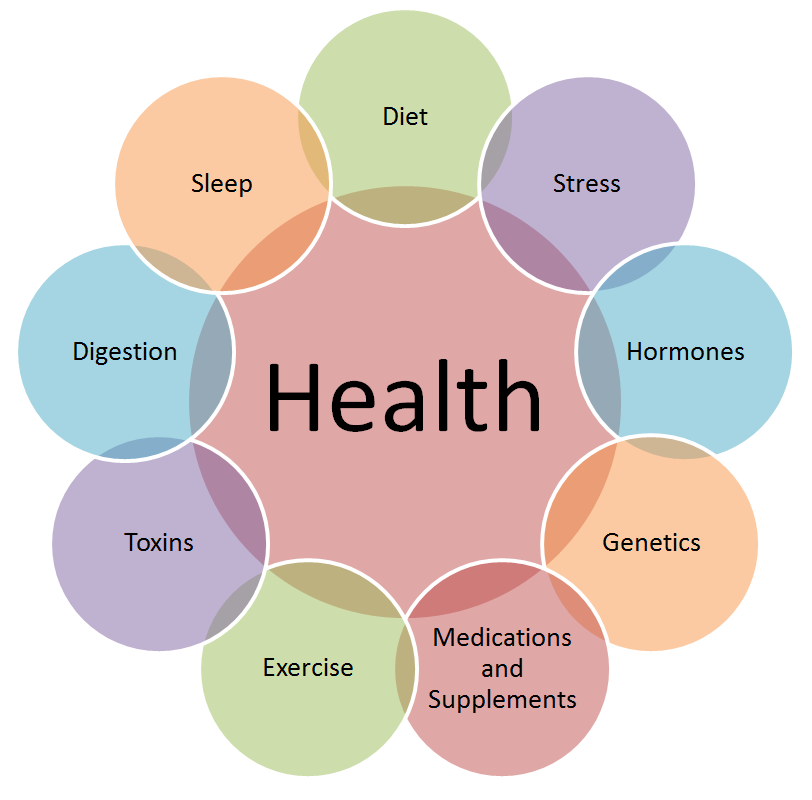
Before diving into immune system boosters, it’s essential to understand how your immune system works. The immune system is a complex network of cells, tissues, and organs that work together to protect your body from harmful invaders like bacteria, viruses, and toxins. Key components include white blood cells, antibodies, the lymphatic system, and the spleen.
When your immune system is strong, it can effectively identify and neutralize threats. However, factors like stress, poor diet, lack of sleep, and sedentary lifestyles can weaken your immunity, making you more susceptible to infections. The good news is that you can take proactive steps to boost your immune system naturally.
Top Natural Immune System Boosters
Here are some of the most effective ways to strengthen your immune system, as recommended by Dr. Zaar:
1. Eat a Balanced, Nutrient-Rich Diet
Your diet plays a crucial role in immune health. Focus on incorporating these immune-boosting foods:
- Citrus Fruits: Oranges, lemons, and grapefruits are rich in vitamin C, which enhances white blood cell production.
- Leafy Greens: Spinach, kale, and broccoli are packed with antioxidants and vitamins A, C, and E.
- Nuts and Seeds: Almonds, sunflower seeds, and walnuts provide vitamin E, a powerful antioxidant.
- Garlic and Ginger: These have natural anti-inflammatory and antimicrobial properties.
- Yogurt and Fermented Foods: Probiotics in yogurt, kefir, and sauerkraut support gut health, which is closely linked to immunity.
2. Stay Hydrated
Water is essential for overall health, including immune function. It helps flush out toxins, transport nutrients, and keep your mucous membranes moist, which acts as a barrier against pathogens. Aim for at least 8-10 glasses of water daily.
3. Get Enough Sleep
Sleep is when your body repairs and regenerates. Lack of sleep can weaken your immune system, making you more prone to infections. Adults should aim for 7-9 hours of quality sleep each night.
4. Exercise Regularly
Moderate exercise, such as walking, yoga, or cycling, can boost your immune system by improving circulation and reducing stress. Aim for at least 30 minutes of physical activity most days of the week.
5. Manage Stress
Chronic stress releases cortisol, a hormone that suppresses immune function. Practice stress-reducing techniques like meditation, deep breathing, or spending time in nature.
6. Take Immune-Boosting Supplements
While a balanced diet should provide most of the nutrients you need, supplements can fill in the gaps. Consider:
- Vitamin D: Supports immune cell function.
- Zinc: Helps fight off infections.
- Elderberry: Known for its antiviral properties.
- Echinacea: May reduce the duration of colds.
7. Avoid Smoking and Limit Alcohol
Smoking and excessive alcohol consumption can weaken your immune system. Quit smoking and limit alcohol to moderate levels to maintain optimal immunity.
8. Practice Good Hygiene
Washing your hands regularly, avoiding close contact with sick individuals, and keeping your surroundings clean can prevent infections and reduce the burden on your immune system.
Lifestyle Changes for Long-Term Immune Health
Boosting your immune system isn’t just about quick fixes; it’s about adopting a healthy lifestyle. Here are some long-term strategies:
1. Maintain a Healthy Weight
Obesity can impair immune function. A balanced diet and regular exercise can help you maintain a healthy weight and boost immunity.
2. Stay Socially Connected
Loneliness and social isolation can negatively impact your immune system. Stay connected with friends and family to support your mental and physical health.
3. Spend Time Outdoors
Sunlight exposure helps your body produce vitamin D, which is essential for immune health. Aim for 15-30 minutes of sunlight daily.
4. Limit Processed Foods
Processed foods are often high in sugar, salt, and unhealthy fats, which can weaken your immune system. Opt for whole, unprocessed foods instead.
Common Myths About Immune System Boosters
There’s a lot of misinformation about immune health. Let’s debunk some common myths:
1. Myth: Supplements Alone Can Boost Immunity
While supplements can help, they’re not a substitute for a healthy diet and lifestyle. Focus on whole foods first.
2. Myth: You Can “Boost” Your Immune System Overnight
Immune health is a long-term commitment. Consistency is key.
3. Myth: Only Vitamin C Matters
While vitamin C is important, other nutrients like zinc, vitamin D, and antioxidants are equally crucial.
When to Seek Medical Advice
While these tips can help strengthen your immune system, it’s important to consult a healthcare professional if you:
- Experience frequent infections.
- Have a chronic medical condition.
- Notice unexplained fatigue or weakness.
Your doctor can provide personalized advice and rule out any underlying issues.
Conclusion
Your immune system is your body’s first line of defense against illness. By adopting a healthy lifestyle, eating a balanced diet, and managing stress, you can naturally boost your immunity and protect your health. Remember, small, consistent changes can make a big difference over time. Stay proactive, stay healthy, and let your immune system work at its best!
Dr. Zaar is a renowned health expert with over 15 years of experience in nutrition and wellness. Follow her for more tips on living a healthy, balanced life.
If you learn more Immune System, Please visit the drzaar.com