Diabetes is a chronic condition that affects millions of people worldwide. While managing blood sugar levels is crucial, preventing complications is equally important. Diabetes can lead to serious health issues such as heart disease, kidney failure, nerve damage, and vision problems. However, with proper endocrinology care, these complications can be prevented or managed effectively. In this article, we’ll explore how endocrinology care plays a vital role in diabetes management and provide actionable tips to help you stay healthy.
Understanding Diabetes and Its Complications
Diabetes occurs when the body cannot produce enough insulin or effectively use the insulin it produces. This leads to elevated blood sugar levels, which, if left unmanaged, can damage various organs and systems in the body. Common complications of diabetes include:
- Cardiovascular Disease: High blood sugar levels can damage blood vessels, increasing the risk of heart attack and stroke.
- Kidney Damage (Nephropathy): Diabetes is a leading cause of kidney failure.
- Nerve Damage (Neuropathy): High blood sugar can damage nerves, leading to pain, numbness, and digestive issues.
- Eye Damage (Retinopathy): Diabetes can cause vision problems and even blindness.
- Foot Problems: Poor circulation and nerve damage can lead to foot ulcers and infections.
The good news is that with proper endocrinology care, these complications can be prevented or delayed.
The Role of Endocrinology Care in Diabetes Management
Endocrinology is the branch of medicine that focuses on hormone-related disorders, including diabetes. An endocrinologist specializes in diagnosing and managing conditions like diabetes, ensuring patients receive personalized care to prevent complications. Here’s how endocrinology care can help:
- Personalized Treatment Plans:
Every patient is unique, and an endocrinologist tailors treatment plans to individual needs. This includes medication, lifestyle recommendations, and regular monitoring. - Advanced Diagnostic Tools:
Endocrinologists use advanced tests to assess blood sugar control, kidney function, and other factors that contribute to diabetes complications. - Comprehensive Care:
Diabetes affects multiple systems in the body, and endocrinologists work with other specialists to provide holistic care. - Education and Support:
Endocrinologists empower patients with knowledge about their condition, helping them make informed decisions about their health.
Key Strategies to Prevent Diabetes Complications
Preventing diabetes complications requires a proactive approach. Here are some key strategies supported by endocrinology care:
1. Monitor Blood Sugar Levels Regularly
Keeping blood sugar levels within the target range is the cornerstone of diabetes management. Regular monitoring helps identify patterns and adjust treatment as needed. Tools like continuous glucose monitors (CGMs) can provide real-time data for better control.
2. Follow a Balanced Diet
A healthy diet is essential for managing diabetes. Focus on:
- Whole grains, fruits, and vegetables
- Lean proteins like fish, chicken, and legumes
- Healthy fats from nuts, seeds, and olive oil
- Limiting processed foods, sugary drinks, and excessive carbohydrates
An endocrinologist or dietitian can help create a meal plan that suits your needs.
3. Engage in Regular Physical Activity
Exercise helps lower blood sugar levels, improve insulin sensitivity, and maintain a healthy weight. Aim for at least 150 minutes of moderate-intensity exercise per week, such as walking, swimming, or cycling.
4. Take Medications as Prescribed
If lifestyle changes alone are not enough, medications like insulin or oral hypoglycemic agents may be necessary. It’s important to take these as prescribed and communicate any side effects to your healthcare provider.
5. Manage Blood Pressure and Cholesterol
High blood pressure and cholesterol levels increase the risk of diabetes complications. Regular monitoring and medications, if needed, can help keep these under control.
6. Quit Smoking and Limit Alcohol
Smoking and excessive alcohol consumption can worsen diabetes complications. Seek support to quit smoking and drink alcohol in moderation, if at all.
7. Schedule Regular Check-Ups
Regular visits to your endocrinologist and other healthcare providers are essential for early detection and management of complications. These check-ups may include:
- Blood tests to monitor HbA1c, kidney function, and cholesterol levels
- Eye exams to detect retinopathy
- Foot exams to check for nerve damage or ulcers
8. Stay Informed and Educated
Knowledge is power when it comes to diabetes management. Attend diabetes education programs, read reliable resources, and stay updated on the latest treatments and technologies.
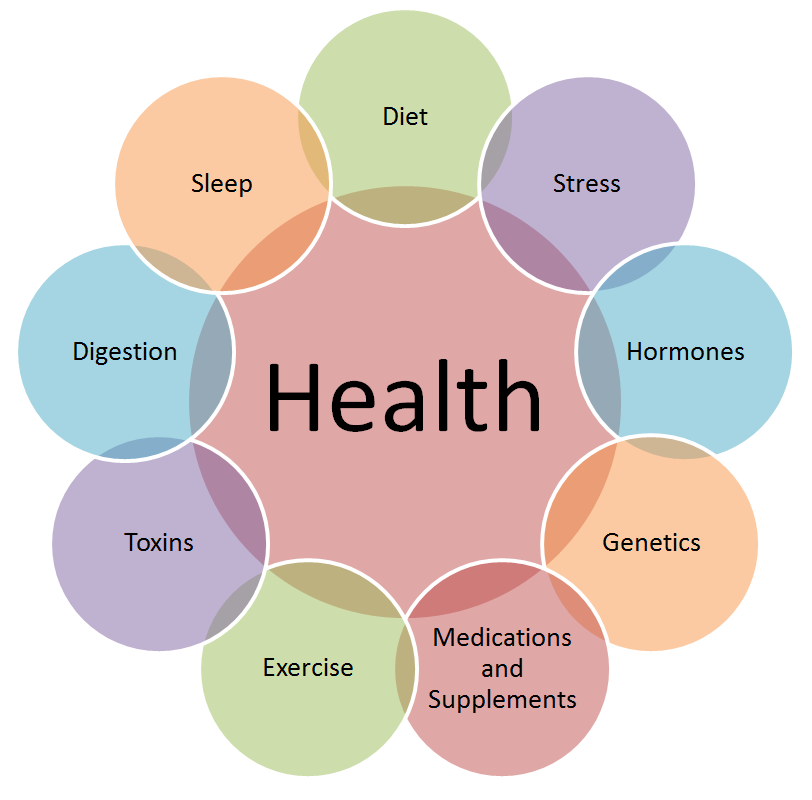
The Importance of a Multidisciplinary Approach
Diabetes care often requires a team of healthcare professionals, including:
- Endocrinologists: Specialize in diabetes and hormone-related disorders.
- Dietitians: Provide guidance on nutrition and meal planning.
- Diabetes Educators: Teach patients how to manage their condition.
- Podiatrists: Care for foot health and prevent complications.
- Ophthalmologists: Monitor eye health and detect retinopathy.
This collaborative approach ensures comprehensive care and reduces the risk of complications.
Technological Advancements in Diabetes Care
Advancements in technology have revolutionized diabetes management. Some of the latest tools include:
- Continuous Glucose Monitors (CGMs): Provide real-time blood sugar readings and trends.
- Insulin Pumps: Deliver insulin continuously, mimicking the body’s natural insulin production.
- Telemedicine: Allows patients to consult with their endocrinologist remotely, improving access to care.
These innovations make it easier to monitor and manage diabetes effectively.
Lifestyle Changes for Long-Term Success
Preventing diabetes complications is not just about medications and doctor visits; it’s also about adopting a healthy lifestyle. Here are some tips:
- Set Realistic Goals: Start with small, achievable changes and build on them over time.
- Stay Consistent: Consistency is key to long-term success in diabetes management.
- Seek Support: Join support groups or connect with others who have diabetes to share experiences and tips.
- Prioritize Mental Health: Managing a chronic condition can be stressful. Practice mindfulness, meditation, or seek counseling if needed.
When to Seek Help
If you experience any of the following symptoms, contact your endocrinologist immediately:
- Persistent high or low blood sugar levels
- Numbness, tingling, or pain in your hands or feet
- Vision changes or eye pain
- Swelling in your legs or feet
- Chest pain or shortness of breath
Early intervention can prevent complications from worsening.
Conclusion
Diabetes is a complex condition, but with proper endocrinology care, complications can be prevented or managed effectively. By monitoring blood sugar levels, adopting a healthy lifestyle, and working closely with your healthcare team, you can take control of your health and live a fulfilling life.
Remember, diabetes management is a lifelong journey, and small, consistent steps can lead to significant improvements. If you or a loved one is living with diabetes, don’t hesitate to seek the guidance of an endocrinologist. Together, you can create a plan that works for you and ensures a healthier future.
If you learn more about Diabetes Complications, Please visit the drzaar.com