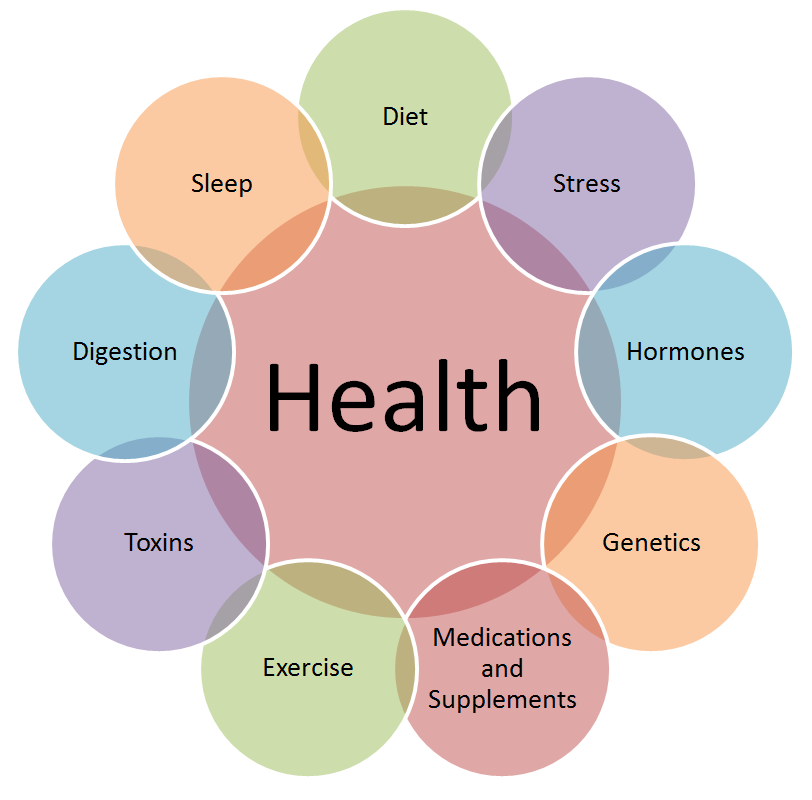
The endocrine system is a complex network of glands that produce and regulate hormones, which control essential bodily functions such as metabolism, growth, reproduction, and mood. When this system is disrupted, it can lead to a wide range of endocrine disorders, including diabetes, thyroid disease, adrenal insufficiency, and polycystic ovary syndrome (PCOS). Early diagnosis of these conditions is critical for effective management and prevention of long-term complications. In this article, we’ll explore the importance of early diagnosis in endocrine disorders, common symptoms to watch for, and the tools and strategies used to detect these conditions promptly.
Why Early Diagnosis Matters
Endocrine disorders often develop gradually, and their symptoms can be subtle or mistaken for other conditions. However, early diagnosis offers several key benefits:
- Preventing Complications:
Many endocrine disorders, if left untreated, can lead to severe complications such as heart disease, kidney failure, nerve damage, and osteoporosis. Early intervention can help prevent or delay these outcomes. - Improving Quality of Life:
Hormonal imbalances can cause debilitating symptoms like fatigue, weight changes, mood swings, and sexual dysfunction. Timely treatment can alleviate these symptoms and restore overall well-being. - Reducing Healthcare Costs:
Early diagnosis and treatment can reduce the need for expensive medical interventions and hospitalizations associated with advanced disease. - Enhancing Treatment Effectiveness:
Many endocrine disorders respond better to treatment when detected early. For example, early management of diabetes can prevent the progression of the disease and reduce the risk of complications.
Common Endocrine Disorders and Their Symptoms
Understanding the symptoms of endocrine disorders is the first step toward early diagnosis. Here are some common conditions and their warning signs:
1. Diabetes
- Frequent urination
- Excessive thirst and hunger
- Unexplained weight loss
- Fatigue
- Blurred vision
2. Hypothyroidism (Underactive Thyroid)
- Fatigue
- Weight gain
- Cold intolerance
- Dry skin and hair
- Depression
3. Hyperthyroidism (Overactive Thyroid)
- Weight loss
- Rapid heartbeat
- Anxiety and irritability
- Heat intolerance
- Tremors
4. Adrenal Insufficiency (Addison’s Disease)
- Fatigue
- Muscle weakness
- Weight loss
- Low blood pressure
- Darkening of the skin
5. Polycystic Ovary Syndrome (PCOS)
- Irregular periods
- Excessive hair growth
- Acne
- Weight gain
- Infertility
6. Cushing’s Syndrome
- Weight gain, particularly around the abdomen
- Moon face (round, red face)
- Thin, fragile skin
- High blood pressure
- Muscle weakness
If you experience any of these symptoms, it’s important to consult a healthcare provider for further evaluation.
Diagnostic Tools for Endocrine Disorders
Early diagnosis of endocrine disorders relies on a combination of clinical evaluation, laboratory tests, and imaging studies. Here are some common diagnostic tools:
- Blood Tests:
Blood tests measure hormone levels and can identify imbalances. For example:- Fasting blood glucose and HbA1c for diabetes
- Thyroid-stimulating hormone (TSH) for thyroid disorders
- Cortisol levels for adrenal disorders
- Urine Tests:
Urine tests can detect abnormal levels of hormones or their metabolites, such as cortisol in Cushing’s syndrome. - Imaging Studies:
Imaging techniques like ultrasound, CT scans, and MRIs can help visualize gland abnormalities, such as thyroid nodules or adrenal tumors. - Stimulation Tests:
These tests assess how glands respond to stimuli. For example, the ACTH stimulation test evaluates adrenal function. - Genetic Testing:
In some cases, genetic testing may be used to identify inherited endocrine disorders, such as multiple endocrine neoplasia (MEN).
The Role of Regular Screenings
Regular health screenings play a vital role in the early detection of endocrine disorders, especially for individuals at higher risk. For example:
- Diabetes: Adults over 45 or those with risk factors like obesity, family history, or sedentary lifestyle should undergo regular blood sugar testing.
- Thyroid Disorders: Women over 60 and those with a family history of thyroid disease should have periodic thyroid function tests.
- Adrenal Disorders: Individuals with unexplained fatigue, weight loss, or skin changes should be evaluated for adrenal insufficiency.
Challenges in Early Diagnosis
Despite the importance of early diagnosis, several challenges can delay detection:
- Non-Specific Symptoms:
Many endocrine disorders present with vague symptoms that can be mistaken for other conditions. - Lack of Awareness:
Patients and healthcare providers may not recognize the signs of endocrine disorders, leading to delayed diagnosis. - Access to Healthcare:
Limited access to healthcare services can prevent individuals from receiving timely evaluations and tests. - Stigma:
Some patients may avoid seeking help due to stigma or embarrassment about their symptoms.
Strategies for Improving Early Diagnosis
To overcome these challenges, the following strategies can be implemented:
- Patient Education:
Raising awareness about the symptoms and risk factors of endocrine disorders can empower individuals to seek help early. - Healthcare Provider Training:
Educating healthcare providers about the signs of endocrine disorders can improve diagnostic accuracy. - Screening Programs:
Implementing routine screening programs for high-risk populations can facilitate early detection. - Telemedicine:
Telemedicine can improve access to healthcare, particularly for individuals in remote or underserved areas. - Multidisciplinary Approach:
Collaboration between endocrinologists, primary care physicians, and other specialists can ensure comprehensive care and timely diagnosis.
The Impact of Early Diagnosis on Treatment Outcomes
Early diagnosis not only improves treatment outcomes but also enhances the overall quality of life for patients. For example:
- Diabetes: Early management through lifestyle changes and medication can prevent complications like neuropathy, retinopathy, and cardiovascular disease.
- Thyroid Disorders: Prompt treatment can alleviate symptoms and prevent long-term issues such as goiter or heart problems.
- Adrenal Insufficiency: Early intervention can prevent life-threatening adrenal crises.
- PCOS: Timely diagnosis and treatment can improve fertility and reduce the risk of metabolic syndrome.
Conclusion
Early diagnosis of endocrine disorders is crucial for effective treatment and prevention of complications. By recognizing the symptoms, undergoing regular screenings, and seeking timely medical care, individuals can take control of their health and improve their quality of life.
If you suspect you may have an endocrine disorder, don’t hesitate to consult a healthcare provider. Remember, early intervention can make all the difference in managing these conditions and ensuring a healthier future.
If you learn more about Endocrine Disorders, Please Visit drzaar.com